PCNs were set out by NHS England (NHSE) as a Directed Enhanced Service (DES) as part of the changes to the GP contract for 19/20 and were originally outlined within the Five-year framework for GP contract reform published on the 31st January 2019. As the framework is a DES, all practices had a contractual right to sign up to the new Primary Care Network DES which commenced in July 2019.
Although this is a DES, it set out a new way of working for practices. Individual practices signed up to the DES but the majority of the funding that is allocated to the DES does not go to the individual practices, but to their PCN as a whole Within 19/20 other funding associated with and paid directly to the PCNs included money to support PCN administration, to fund a Clinical Director (9 months funding) and to fund one Clinical Pharmacist (70% funded) and one Social Prescriber (100% funded) on recruitment to the posts (up to 9 months funding) as part of the Additional Roles Reimbursement Scheme (ARRS).
In 20/21 the agreement was revised, with key points being:
- Major enhancements to the Additional Roles Reimbursement Scheme to help secure 26,000 additional staff
- A raft of measures to aid GP recruitment and retention to help deliver 6000 more doctors working in primary care
- Improvements in access for patients: More people working in general practice will help achieve 50 million more appointments in general practice
- Further improvements to the Quality and Outcomes Framework
- Reforms to vaccinations and immunisations payment arrangements to improve vaccination coverage
- A new universal 6-8 week post-natal check for new mothers
- Three new services in 20/21: Structured Medication Review and Medicines Optimisation, Enhanced Health in Care Homes and Supporting Early Cancer Diagnosis service.
- New incentives under the Investment and Impact Fund to increase uptake of learning disability health checks, seasonal flu jabs, social prescribing referrals, and improve specific aspects of prescribing.
In the following three years of the DES, further funding is being made available to PCNs around ARRS, Enhanced Access, investment and impact fund and seven national service specifications related to: 1) structured medication reviews and optimisation; 2) enhanced health in care homes; 3) anticipatory care; 4) supporting early cancer diagnosis; 5) personalised care; 6) CVD prevention and diagnosis; 7) tackling neighbourhood inequalities.
The CCG has been very clear that the funding identified via the PCN DES is for practices (where applicable) and the PCNs. This DES is part of the GP contract and we are starting to see real progress in PCNs in Bradford and getting established ways of working embedded.
Each PCN has a Clinical Director using the funding allocated to them (based on per registered patient). The role of the PCN Clinical Director is specified by NHSE and includes:
- The Clinical Director will work collaboratively with Clinical Directors from other PCNs within the ICS/STP area, playing a critical role in shaping and supporting their ICS/STP, helping to ensure full engagement of primary care in developing and implementing local system plans.
- They will support PCN implementation of agreed service changes and pathways and will work closely with member practices and the commissioner and other networks to develop, support and deliver local improvement programmes aligned to national priorities.
- They will develop local initiatives that enable delivery of the PCN’s agenda, working with commissioners and other networks to reflect local needs and ensuring initiatives are coordinated.
- They will develop relationships and work closely with other Clinical Directors, clinical leaders of other primary care, health and social care providers, local commissioners and LMCs.
The PCN Clinical Directors fulfil much of the above by working within the model of the 10 Community Partnerships and 3 Localities across Bradford.
BCA, PCNs and CPs
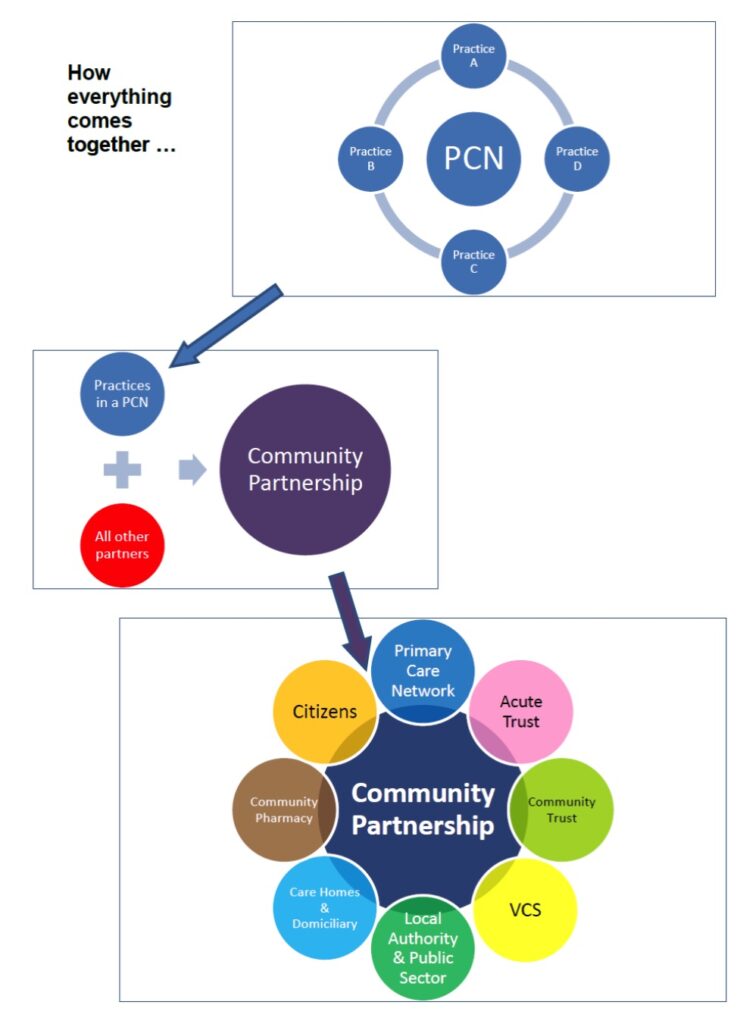
BCA and the wider system are clear that the PCNs will not ‘take over’ the CPs, but that they are an important and equal partner around the table as depicted in the image below. This meets the needs of the PCN in regards to delivery of the DES, but also meets the needs of wider system working and transformation as our CPs are the building blocks from which our integrated care system will continue to grow.
Due to CPs and PCNs being two different entities, the Chair of the CP does not need to be the Clinical Director of the PCN, even if the footprints they are working across are the same. The Clinical Director would be expected to fully participate in the CP meetings as the PCN is a critical player within the CP, but they do not also need to be the Chair of the CP (unless that is agreed by all the CP partners).
BCA facilitates a monthly meeting of the 10 Bradford Clinical Directors and our neighbouring CDs in Airedale, with acknowledgement that this is increasingly the vehicle for Primary Care representation in the emerging system. The group will continue to work together to put ideas forward to take back some control before any new approaches are imposed upon primary care.